Ever imagined trying to breathe but feeling like your lungs are filled with concrete? For patients on ventilators, this is a harsh reality. Their life depends on a machine breathing for them, and nurses are the vital link between the patient and their respiratory lifeline. Understanding the complexities of ventilator care and creating effective nursing care plans is critical to ensure the best possible outcomes for these patients.
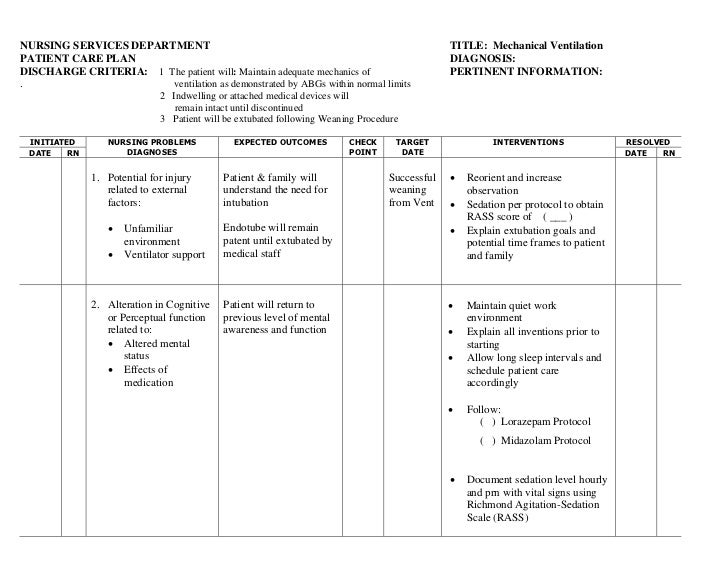
Image: www.slideshare.net
This article will dive deep into the world of nursing care plans for ventilator patients. We’ll unpack the crucial elements of these plans, explore the challenges nurses face, and provide practical strategies for successful care. Plus, we’ll make it easy by offering a free downloadable PowerPoint template designed to help you create comprehensive and tailored care plans. Let’s begin!
Understanding Ventilators and Their Role in Patient Care
What is a Ventilator?
Imagine your lungs as a pump, taking in fresh air and expelling carbon dioxide. A ventilator acts as a mechanical pump, taking over this crucial function when your own lungs can’t keep up. It delivers oxygen-rich air into the airways and removes carbon dioxide.
Types of Ventilators
Ventilators come in a variety of shapes and sizes, each with different features and purposes.
- Mechanical Ventilators: These are the mainstay of critical care, used for patients with acute respiratory failure. They deliver breaths at precise volumes and pressures, often with the help of sophisticated algorithms.
- Non-Invasive Ventilators: These use masks or nasal prongs to provide assisted breathing without the need for an endotracheal tube. They are often used for patients with mild to moderate respiratory failure.
- Home Ventilators: These are portable and allow patients to live independently with chronic respiratory conditions.
Image: www.slideshare.net
Why is Nursing Care Planning Essential for Ventilator Patients?
Ventilator patients face a unique set of challenges, requiring highly specific and individualized interventions. Here’s why nursing care plans are critical:
- Complexity of care: Ventilator management involves monitoring multiple vital signs, adjusting settings, and addressing potential complications. Comprehensive care plans help nurses stay organized and ensure no crucial aspect of care is overlooked.
- Patient safety: Ventilator-associated complications, such as pneumonia and lung injury, are significant risks. Effective care plans with detailed protocols and monitoring strategies help minimize these risks.
- Communication and teamwork: Nursing care plans are essential for clear communication between nurses, doctors, and other healthcare professionals involved in the patient’s care. This shared understanding promotes coordinated efforts and optimal patient care.
- Patient empowerment and education: Care plans can include strategies for patient engagement and education, enabling patients (or their families) to understand their condition, treatment, and role in their recovery.
Key Components of a Nursing Care Plan for Ventilator Patients
1. Patient Assessment: The Foundation of Effective Care
The first step in crafting a care plan is a thorough patient assessment. This involves gathering essential information about the patient’s:
- Medical history: Previous respiratory illnesses, allergies, medications, and overall health status.
- Current condition: Reason for ventilation, severity of respiratory failure, level of consciousness, and overall clinical status.
- Vital signs: Temperature, heart rate, blood pressure, oxygen saturation, and respiratory rate.
- Respiratory assessment: Lung sounds, chest movement, cough, and sputum production.
- Psychosocial assessment: The patient’s emotional state, coping mechanisms, and support systems.
2. Goals of Ventilator Management
Once you understand the patient’s needs and limitations, it’s time to establish clear goals for ventilator management. These goals might include:
- Maintaining adequate oxygenation: Ensuring the patient receives enough oxygen to maintain vital functions and prevent tissue damage.
- Preventing respiratory complications: Minimizing the risk of pneumonia, atelectasis (collapsed lung), and other lung injuries.
- Weaning from ventilation: Gradually transitioning the patient back to independent breathing.
- Providing psychosocial support: Addressing the patient’s emotional needs and providing comfort during their stay on the ventilator.
3. Nursing Interventions and Strategies
This section outlines the specific actions that you, the nurse, will take to achieve the stated goals.
- Monitoring vital signs: Continuously monitoring respiratory rate, oxygen saturation, heart rate, and blood pressure.
- Ventilator management: Adjusting ventilator settings as needed based on patient response, monitoring alarms for changes in pressure or flow, and providing appropriate sedation and pain management.
- Respiratory care: Performing chest physiotherapy, suctioning the airway, and providing humidified oxygen.
- Positioning: Positioning the patient for optimal lung expansion and drainage, encouraging mobility within the limits of their condition.
- Infection control: Maintaining strict hand hygiene, using sterile techniques for procedures, and implementing isolation precautions when necessary.
- Psychosocial support: Providing emotional support, addressing anxiety and fear, and communicating openly with the patient and family.
4. Evaluation: Measuring Progress
It’s crucial to monitor the patient’s progress and make adjustments to the care plan if needed. This involves:
- Monitoring for effectiveness: Regularly reviewing the patient’s vital signs, respiratory status, and response to interventions.
- Evaluating outcomes: Determining if the care plan is meeting the established goals.
- Assessing for complications: Identifying any potential problems, such as airway obstruction, ventilator-associated pneumonia, or lung injury.
- Communicating with healthcare team: Sharing updates and progress with the physician, respiratory therapist, and other members of the care team.
Practical Tips for Creating Effective Nursing Care Plans for Ventilator Patients
- Individualize: Each patient’s needs are unique. Tailor the care plan to the individual’s condition, medical history, and goals.
- Collaborate: Work closely with the physician, respiratory therapist, and other healthcare professionals to ensure a cohesive plan.
- Be specific: Use clear and concise language to document nursing interventions, providing detailed protocols and instructions for other team members.
- Prioritize patient engagement: Explain the care plan to the patient in a way they can understand, answer their questions, and involve them in the decision-making process as much as possible.
- Document everything: Thorough documentation is crucial for tracking progress, identifying trends, and ensuring continuity of care.
Download Your Free Nursing Care Plan Template (PPT)
To help you get started, we’ve developed a free and customizable PowerPoint template designed specifically for nursing care plans for ventilator patients. Click here to download your free template. It includes detailed sections for:
- Patient Demographics
- Medical History
- Current Condition
- Vital Signs
- Respiratory Assessment
- Goals of Ventilator Management
- Nursing Interventions
- Monitoring and Evaluation
- Patient Education
- Family Communication
Nursing Care Plan Of Patient On Ventilator Ppt
Conclusion: Elevating Ventilator Care Through Effective Nursing Plans
Caring for ventilator patients is a complex and challenging task. By crafting thorough and individualized nursing care plans, you can provide the best possible care, ensure patient safety, and empower both the patient and their family. Remember, consistent assessment, clear goals, and effective monitoring are the cornerstones of successful ventilator management. Use this article and the free template to enhance your skills and elevate the standard of care for your ventilator patients!






