Imagine a bustling city where traffic is at a standstill. Cars are gridlocked, unable to reach their destinations, and the flow of goods and services is disrupted. Now, imagine your body as a city. The arteries are the roads, the blood is the traffic, and the tissues are the businesses and individuals that rely on this constant flow for survival. When the blood flow is compromised, the tissues suffer. This is what happens when ineffective tissue perfusion occurs.
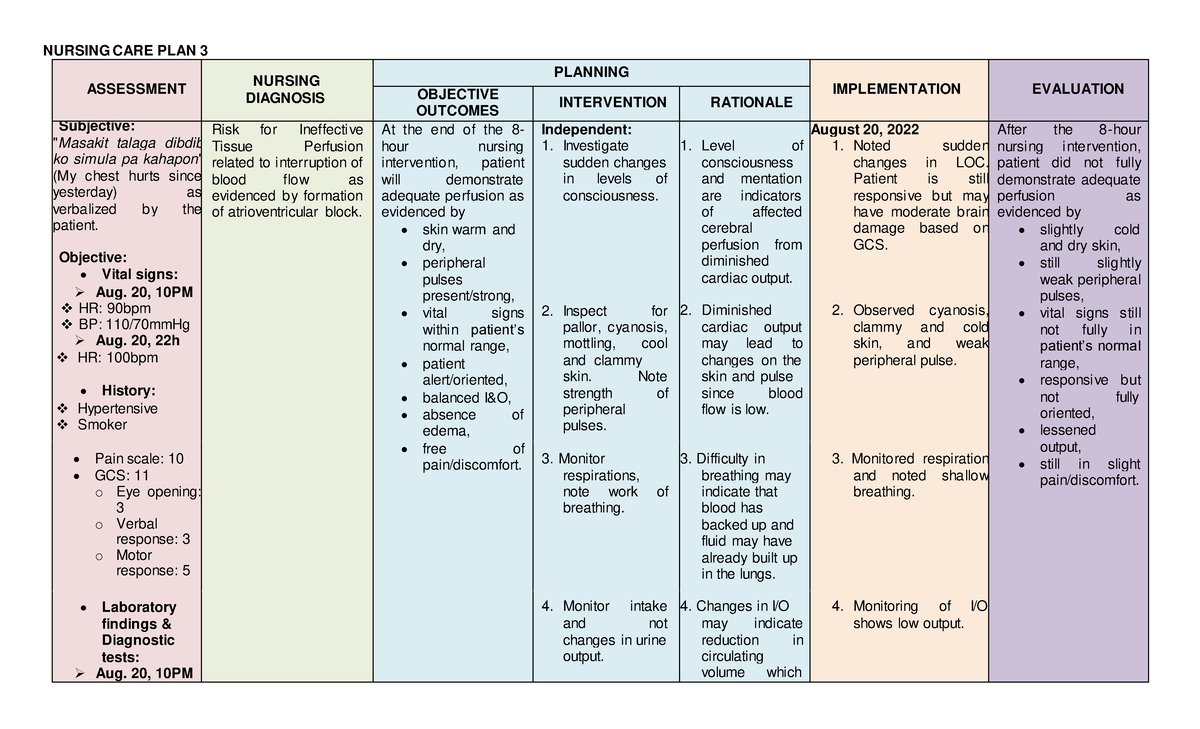
Image: www.studocu.com
Ineffective tissue perfusion is a condition where blood flow to the tissues is inadequate. This can be caused by a variety of factors, including circulatory problems, heart disease, and even prolonged immobility. Understanding this condition and developing effective nursing care plans is crucial for nurses to ensure the well-being of their patients. In this article, we will delve deeper into the intricacies of ineffective tissue perfusion, exploring its causes, assessing its impact, and outlining comprehensive nursing care plans to optimize blood flow and promote tissue health.
Understanding Ineffective Tissue Perfusion
Before we delve into the care plan, it’s essential to understand the underlying processes involved. Ineffective tissue perfusion occurs when the blood flow to tissues is insufficient to meet their metabolic demands. This can be caused by a variety of factors, including:
Causes of Ineffective Tissue Perfusion
- Cardiovascular diseases: Conditions like coronary artery disease, heart valve disorders, and arrhythmias can disrupt blood flow to vital organs.
- Peripheral Vascular Disease (PVD): Narrowing or blockage of blood vessels in the legs and arms can lead to impaired tissue perfusion in these extremities.
- Thromboembolism: Blood clots that travel through the bloodstream and block blood vessels can lead to a sudden and severe reduction in blood flow.
- Hypovolemia: A significant decrease in blood volume due to blood loss or dehydration can result in insufficient blood flow throughout the body.
- Immobility: Prolonged bed rest or inactivity can lead to blood pooling in the legs, causing reduced blood flow back to the heart.
Assessing the Impact: Signs and Symptoms
Recognizing the signs and symptoms of ineffective tissue perfusion is crucial for early intervention and preventing serious complications. Common signs and symptoms can vary depending on the area affected, but some frequent presentations include:
- Pain: Tissues deprived of oxygen often experience pain, which may worsen with activity. This pain may be described as a cramping, burning, or tightness.
- Changes in Skin Color: The skin may appear pale or cyanotic (blue-tinged) in areas with reduced blood flow.
- Changes in Temperature: The affected area may feel cool or cold to the touch.
- Edema: Swelling in the affected area due to fluid buildup from slowed circulation.
- Changes in Sensation: Numbness, tingling, or a pins-and-needles sensation may be experienced due to impaired nerve function.
- Pulselessness: Weak or absent pulses in the affected area indicate a significant reduction in blood flow.
- Delayed Capillary Refill: When pressure is applied to the skin, it should return to its normal color quickly. A slow return to color indicates poor circulation.
- Altered Mental Status: In cases of severe tissue perfusion issues, the brain can be affected, leading to confusion, disorientation, or even coma.

Image: www.coursehero.com
The Importance of Early Detection
Effective tissue perfusion is essential for a variety of bodily functions, including:
- Oxygen Delivery: Blood carries oxygen to the tissues, which is essential for cellular metabolism and energy production.
- Nutrient Transport: Blood delivers nutrients like glucose and amino acids to cells for growth and repair.
- Waste Removal: Blood carries waste products like carbon dioxide and metabolic byproducts away from the tissues.
- Immune System Function: Blood carries white blood cells and other components of the immune system that help fight infections.
When blood flow is compromised, these vital functions are disrupted. This can lead to a range of health problems, including:
- Tissue Death (Necrosis): Without adequate blood flow, tissues can die due to lack of oxygen and nutrients. This is particularly dangerous in organs like the heart and brain, where prolonged oxygen deprivation can lead to irreversible damage.
- Wound Healing Delay: Adequate blood flow is essential for wound healing. Poor circulation can hinder the delivery of healing factors and slow down the repair process.
- Increased Infection Risk: Reduced blood flow weakens the immune system’s ability to fight infections, making individuals more susceptible to infections.
- Amputation: In severe cases, tissue death and infection can lead to amputation of the affected limb.
The severity of ineffective tissue perfusion can vary depending on the underlying cause and the area affected. Prompt recognition and intervention are crucial to prevent serious health complications.
Nursing Care Plan for Ineffective Tissue Perfusion: A Comprehensive Approach
The nursing care plan for ineffective tissue perfusion focuses on optimizing blood flow and preventing further complications. It involves a multi-faceted approach that addresses the patient’s individual needs and promotes healing:
1. Assessment: A Foundation for Effective Care
The first step in developing a nursing care plan is a thorough assessment of the patient’s condition. This involves a detailed history, physical examination, and review of relevant laboratory and diagnostic tests. The nurse should inquire about the patient’s past medical history, current medications, and any recent injuries or surgeries. The physical assessment should focus on:
- Cardiovascular Status: Assess heart rate, rhythm, and blood pressure. Listen for any abnormal heart sounds.
- Peripheral Circulation: Evaluate pulses in all extremities. Look for any signs of edema, skin discoloration, or temperature changes.
- Respiratory Status: Observe breathing rate, depth, and effort. Assess for any signs of dyspnea (difficulty breathing).
- Pain Assessment: Determine the location, intensity, and character of pain. Use a pain scale to objectively measure pain levels.
- Neurological Status: Assess for any changes in level of consciousness, orientation, or neurological function.
- Fluid Status: Assess fluid intake and output. Observe for any signs of dehydration or volume overload.
2. Monitoring: Keeping a Close Watch
Once the initial assessment is complete, ongoing monitoring is crucial to track the patient’s progress and adjust the care plan as needed. Frequent assessments of vital signs, pain levels, and peripheral circulation are essential. Monitoring may include:
- Pulse Oximetry: Measures the oxygen saturation levels in the blood.
- Electrocardiogram (ECG): Records the electrical activity of the heart, helping to identify any abnormalities.
- Blood Pressure: Regular monitoring helps assess the effectiveness of medications and intervention.
- Capillary Refill: Checks the blood flow to the extremities.
- Urine Output: Indicates fluid balance and kidney function.
Recording and documenting all assessments and interventions is essential for maintaining accurate patient records and ensuring continuity of care.
3. Medication Administration: Supporting Circulation
Depending on the underlying cause of ineffective tissue perfusion, medication administration may be a key component of the nursing care plan. The nurse should be aware of the medications prescribed and their potential side effects. Common medications include:
- Anticoagulants: Medications that prevent blood clots, such as heparin and warfarin.
- Antiplatelet Agents: Medications that prevent platelets from sticking together and forming clots, such as aspirin and clopidogrel.
- Vasodilators: Medications that expand blood vessels, improving blood flow, such as nitrates and calcium channel blockers.
- Diuretics: Medications that help remove excess fluid from the body, reducing edema.
- Pain Medications: To manage pain associated with tissue ischemia.
The nurse should monitor the patient’s response to medication, watch for any adverse effects, and promptly report any concerns to the physician.
4. Lifestyle Modifications: Cultivating Healthy Habits
Lifestyle modifications can play a significant role in improving circulation and preventing complications. The nurse should counsel the patient on the following suggestions:
- Smoking Cessation: Smoking damages blood vessels and increases the risk of cardiovascular disease.
- Regular Exercise: Physical activity strengthens the heart and improves blood flow.
- Weight Management: Obesity puts extra strain on the heart and circulatory system.
- Healthy Diet: A diet rich in fruits, vegetables, and whole grains can lower cholesterol levels and improve cardiovascular health.
- Stress Management: Stress can constrict blood vessels and increase the risk of heart disease.
It’s important to empower patients to make positive lifestyle changes and provide them with resources and support to help them achieve their goals.
5. Positional Changes: Promoting Circulation
Positioning the patient correctly can help improve circulation and prevent blood pooling in the legs. Encourage the patient to:
- Elevate the Legs: Elevating the legs above the heart can help improve venous return and reduce swelling.
- Avoid Crossing Legs: Crossing the legs can restrict blood flow and increase the risk of deep vein thrombosis (DVT).
- Frequent Position Changes: Encourage the patient to change positions frequently to prevent pressure on blood vessels and promote circulation.
6. Compression Therapy: Enhancing Venous Return
Compression therapy involves using stockings or bandages to apply pressure to the legs, helping to improve venous return and prevent blood pooling. This can be particularly helpful for patients with PVD or those at risk for DVT.
The nurse should ensure that compression stockings are properly sized and fitted to avoid restricting circulation.
7. Ambulation and Mobility: Relieving Stasis
Encourage early ambulation and mobility as soon as the patient’s condition allows. This helps to prevent blood pooling in the legs, improve circulation, and reduce the risk of complications.
Assist the patient with getting out of bed and moving around safely, providing appropriate support and guidance.
8. Wound Care: Protecting Compromised Skin
Patients with ineffective tissue perfusion are at an increased risk for skin breakdown and wound development. Provide meticulous wound care to prevent infection and promote healing.
- Clean and Dress Wounds: Regularly clean and dress wounds with appropriate dressings and solutions.
- Monitor Wound Healing: Assess the wound for any signs of infection, such as redness, swelling, or drainage.
- Skin Care: Maintain skin hygiene. Keep the skin clean and dry. Moisture can compromise skin integrity.
9. Patient Education: Empowering Self-Care
Providing comprehensive patient education is vital for empowering patients to manage their condition effectively. The nurse should teach the patient about:
- Causes of Ineffective Tissue Perfusion: Help the patient understand the factors that contribute to their condition.
- Signs and Symptoms: Teach the patient how to recognize the early signs of worsening circulation.
- Medication Management: Explain the purpose and potential side effects of their medications.
- Lifestyle Modifications: Encourage the patient to adopt healthy habits that can improve circulation.
- Follow-Up Care: Stress the importance of regular follow-up appointments to monitor their progress.
Nurses play a key role in educating patients about their condition and empowering them to make informed decisions about their health.
Nursing Care Plan For Ineffective Tissue Perfusion
Conclusion: Making a Difference in Patient Care
Ineffective tissue perfusion is a serious condition that requires comprehensive nursing care to optimize blood flow and prevent further complications. By diligently assessing patients, monitoring their progress, and implementing evidence-based interventions, nurses can make a significant difference in improving patient outcomes. Remember that every patient is unique, and the care plan should be individualized to meet their specific needs. The ultimate goal is to provide compassionate, patient-centered care with a focus on promoting healing and maximizing quality of life.






