Imagine waking up feeling tired, your stomach rumbling, but instead of excitement, you feel a dull ache. You’re not hungry. You’re not even remotely interested in food. This is the reality for many patients, and for nurses, it’s a crucial area of concern. Loss of appetite, also known as anorexia, is a complex phenomenon with various underlying causes. It can be a symptom of physical illness, a side effect of medication, a consequence of emotional distress, or even a sign of a more serious condition. Whatever the cause, loss of appetite can significantly impact a patient’s overall health and well-being.
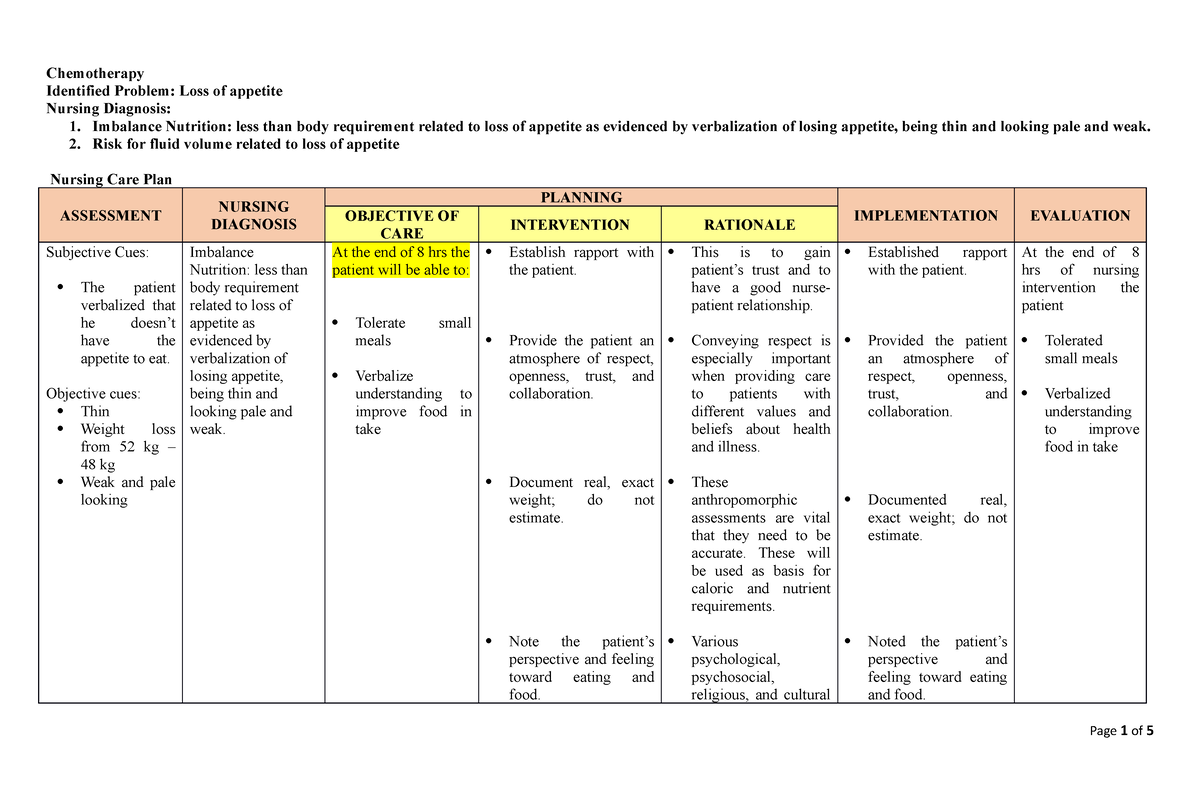
Image: www.studocu.com
This article dives into the intricate world of nursing care plans for loss of appetite. We will explore the various causes behind this symptom, delve into strategies for assessment and diagnosis, and illuminate the specific interventions and nursing care that can help patients regain their appetite and improve their nutritional status. By understanding both the multifaceted nature of this issue and the holistic strategies employed by nurses, we aim to empower you with valuable insights and practical knowledge to address this common concern in patient care.
Understanding Loss of Appetite: A Deeper Dive
The Multifaceted Nature of Loss of Appetite
Loss of appetite is not simply a matter of “not feeling hungry.” It’s a complex symptom that can stem from a variety of factors, often intertwined and affecting one another. These factors can be broadly categorized as:
- Physiological: Patients experiencing illness, chronic pain, or side effects from medications might have a decreased appetite. Certain medical conditions, such as cancer, HIV, or gastrointestinal disorders, can also contribute to loss of appetite.
- Psychological: Mental health conditions like depression, anxiety, and stress can significantly impact eating habits. Grief, trauma, and other emotional factors also play a role.
- Social: Social isolation, financial difficulties, and lack of access to healthy food options can contribute to poor nutrition and loss of appetite.
The Importance of Addressing Loss of Appetite
Neglecting loss of appetite is not an option. It can lead to a cascade of negative consequences, including:
- Malnutrition: Insufficient intake of essential nutrients can weaken the immune system, delay wound healing, and compromise overall health.
- Weight Loss: Unintentional weight loss can be a sign of a serious underlying medical condition.
- Muscle Wasting: The body can start breaking down muscle tissue for energy, leading to weakness and frailty.
- Fatigue: Lack of energy and vitality can affect daily functioning and overall quality of life.
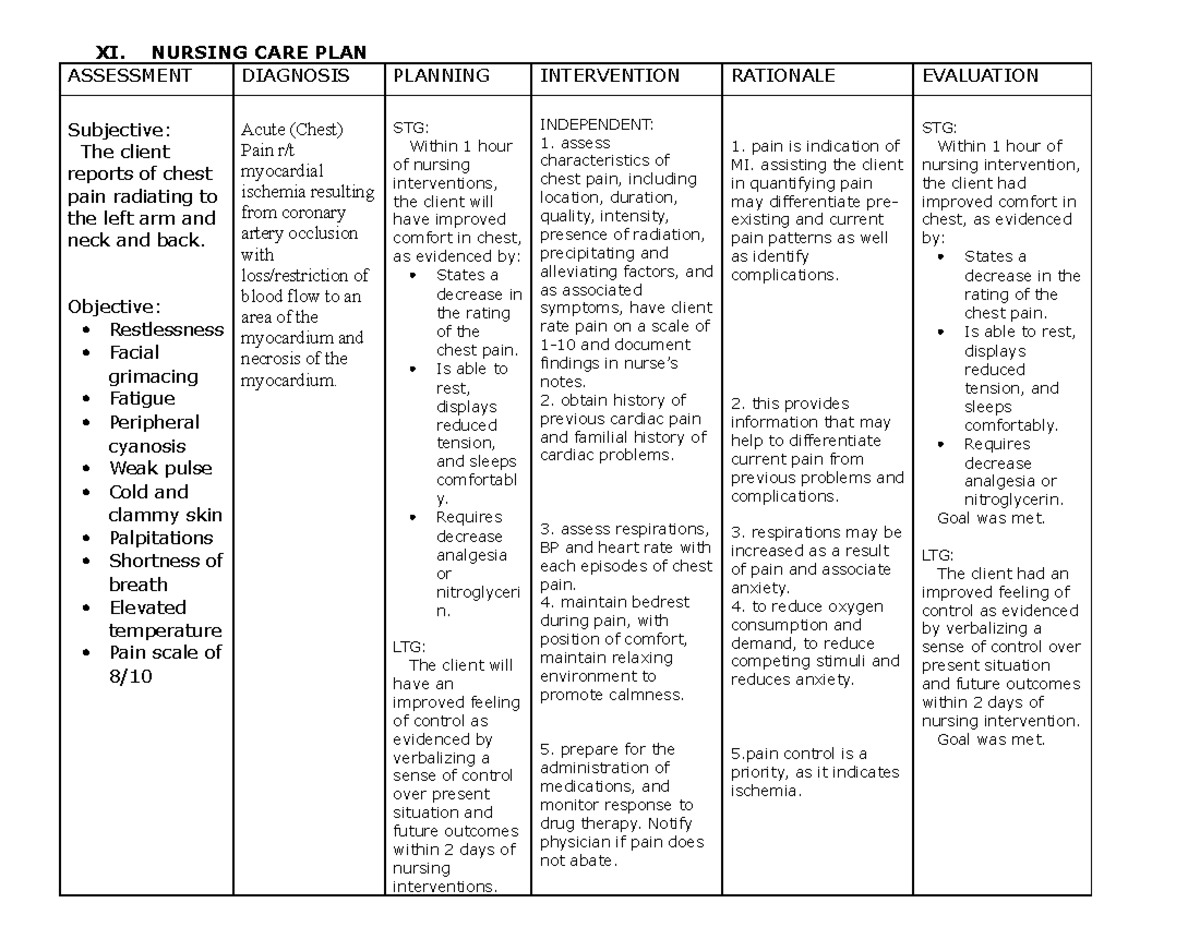
Image: www.myxxgirl.com
Nursing Care Plan: A Step-by-Step Approach
1. Assessment: Identifying the Underlying Cause
The first step in a nursing care plan for loss of appetite is a thorough assessment. Nurses conduct a comprehensive evaluation, gathering information about the patient’s:
- Medical History: Understanding past diagnoses, current medication, and any co-existing conditions is crucial.
- Nutritional Habits: Exploring dietary intake, food preferences, and any recent changes in eating patterns provides valuable insights.
- Emotional and Social Factors: Assessing mood, stress levels, social support network, and financial situation offers a holistic perspective.
- Physical Examination: Observing for signs of dehydration, malnutrition, skin lesions, and weight loss aids in comprehensive assessment.
2. Diagnosis: Defining the Problem
Based on the assessment findings, nurses can formulate a nursing diagnosis. Some common diagnoses associated with loss of appetite include:
- Imbalanced Nutrition: Less than Body Requirements – This diagnosis is applicable when the patient’s intake is insufficient to meet their nutritional needs.
- Impaired Oral Mucous Membrane – This diagnosis applies when the patient has difficulty eating due to mouth sores or inflammation.
- Activity Intolerance – This diagnosis applies if the patient experiences fatigue and weakness due to poor nutrition, making it challenging for them to participate in daily activities.
3. Planning: Establishing Goals and Interventions
The nursing care plan focuses on achieving specific and measurable goals, such as:
- Improving Nutritional Intake: Increasing daily caloric intake to meet the patient’s nutritional requirements.
- Maintaining Weight: Preventing further weight loss or promoting gradual weight gain.
- Improving Energy Levels: Enhancing the patient’s stamina and ability to participate in daily activities.
- Addressing Underlying Causes: Addressing the root cause of the loss of appetite to promote lasting change.
To achieve these goals, nurses employ a range of interventions, including:
- Nutritional Counseling: Providing dietary advice and recommendations, ensuring adequate intake of essential nutrients. This can involve collaborating with a registered dietitian to create personalized meal plans.
- Medication Management: Addressing the potential side effects of medication that may contribute to loss of appetite, working closely with the physician to adjust dosages or consider alternative medications.
- Symptom Management: Addressing nausea, vomiting, pain, and other symptoms that may discourage eating.
- Environmental Modifications: Creating a comfortable and inviting eating environment, ensuring adequate lighting, reducing distractions, and offering support during mealtimes.
- Social Support: Encouraging family and friends to provide emotional support and assist with meal preparation.
- Behavioral Therapies: Employing stress reduction techniques, mindfulness exercises, and cognitive behavioral therapy to address underlying psychological factors.
- Complementary Therapies: Exploring alternative therapies like acupuncture, aromatherapy, or massage to potentially improve appetite and overall well-being.
4. Implementation: Putting the Plan into Action
Once the care plan is established, nurses implement the interventions and closely monitor the patient’s progress. This involves:
- Frequent Monitoring: Regularly assessing the patient’s weight, intake, symptoms, and overall well-being.
- Medication Administration: Ensuring timely and accurate administration of medications prescribed to address loss of appetite or associated symptoms.
- Mealtime Assistance: Offering support during meals, providing assistance with feeding if needed, and creating a pleasant and comfortable environment.
- Patient Education: Providing information about nutrition, healthy eating habits, and strategies for managing loss of appetite.
5. Evaluation: Assessing the Effectiveness
Nurses continuously evaluate the effectiveness of the care plan and modify it based on the patient’s progress. This includes:
- Analyzing Data: Reviewing the patient’s weight, intake records, symptom reports, and other relevant data to gauge improvement.
- Patient Feedback: Regularly checking in with the patient to understand their perspectives, experiences, and challenges.
- Reassessing Needs: Adjusting the care plan as needed based on the patient’s changing needs and response to interventions.
Empowering Patients to Regain Their Appetite
The ultimate goal of a nursing care plan for loss of appetite is to empower patients to regain control over their eating habits and regain a sense of well-being. By combining a comprehensive assessment, tailored interventions, and ongoing monitoring, nurses play a vital role in helping patients:
- Identify and Address the Underlying Cause: Whether it’s a medical condition, medication side effect, or emotional distress, nurses work to identify the root cause and create a plan for effective management.
- Improve Their Nutritional Status: By promoting healthy eating habits, providing nutritional counseling, and adjusting medication if necessary, nurses help patients achieve adequate nutrient intake and improve their overall health.
- Gain Confidence and Control: Through a collaborative approach, patients develop a sense of agency and empowerment, leading to increased self-efficacy in managing their loss of appetite.
Nursing Care Plan For Loss Of Appetite
Conclusion: A Journey of Hope and Recovery
Loss of appetite is a complex issue that requires a multi-faceted approach involving careful assessment, targeted interventions, and ongoing monitoring. By providing compassionate and patient-centered care, nurses empower individuals to regain their appetite and improve their overall health. Remember, working closely with a healthcare professional is essential for addressing the underlying cause and developing the most effective care plan. We encourage you to engage in open communication with your doctor or nurse, share your concerns, and actively participate in your own recovery. Together, we can navigate this journey of hope and recovery.






